In today’s competitive healthcare landscape, Mental Health Provider Credentialing Services play a crucial role in ensuring that mental health professionals meet all necessary standards and regulations. These services streamline the complex process of verifying licenses, education, work experience, and professional references, allowing providers to focus on delivering quality care to their patients. By utilizing Mental Health Provider Credentialing Services, clinics and private practices can maintain compliance with insurance companies, reduce administrative burdens, and accelerate the onboarding process for new practitioners, ultimately improving operational efficiency and patient satisfaction.
Insurance credentialing is the gateway for mental health providers to participate in insurance networks, receive reimbursements, and establish credibility with patients. Without credentialing, therapists, counselors, psychologists, and other mental health professionals are limited to self-pay clients. In Tier One markets such as the USA, UK, Canada, and Australia, insurance coverage is central to patient decisions, making credentialing an indispensable part of professional practice.
For providers, the process is often frustrating. Applications can take months, require multiple follow-ups, and vary significantly depending on state regulations and insurance companies. The pain points include delays in approval, rejection due to incomplete paperwork, and maintaining multiple CAQH (Council for Affordable Quality Healthcare) profiles when practicing across different states. These challenges can lead to lost revenue and patient attrition.
However, credentialing also offers a powerful promise: improved access to patient populations, higher trust from clients, and consistent revenue streams through insurance reimbursements. By understanding and navigating the credentialing process effectively, mental health professionals can maximize their ROI, build sustainable practices, and scale their services with confidence. This guide provides a step-by-step breakdown of the credentialing journey, with region-specific insights for Tier One countries, practical checklists, and strategies to optimize lead generation through credentialing.
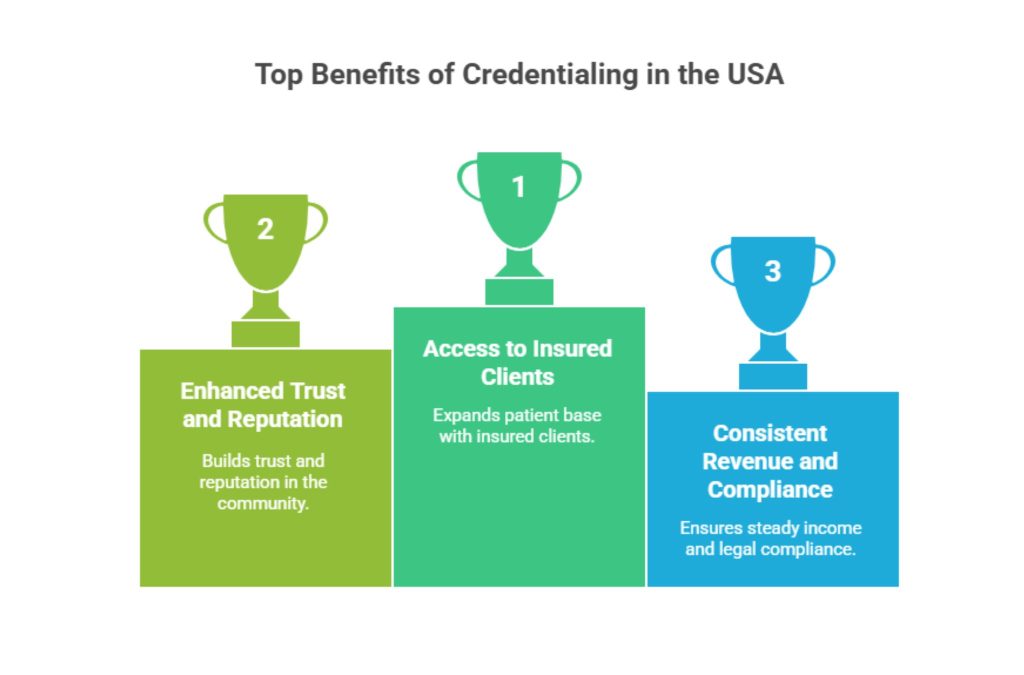
Why Credentialing Matters for Mental Health Providers in the USA
Credentialing is not just a compliance requirement—it is a growth strategy for therapists and mental health practices. In the United States, insurance companies rely on credentialing to verify a provider’s qualifications, licenses, and professional background. Being on an insurance panel opens access to insured clients, who are often the majority in competitive urban markets.
A 2024 survey of private practices in the U.S. revealed that credentialed therapists see 45% more patient bookings compared to non-credentialed providers. Patients trust the credibility of insurance-approved professionals, while practices gain steady revenue through reimbursements. For group practices, credentialing is a strategic move to scale, since new hires must also undergo the process.
| Key Benefits of Credentialing in the USA | Impact |
| Access to insured client base | 2x increase in patient intake |
| Higher trust and reputation | Stronger community presence |
| Insurance reimbursements | Consistent monthly revenue |
| Compliance with state laws | Avoids penalties and restrictions |
Case Study:
A Chicago-based counseling center reported a 60% revenue increase within 12 months after completing credentialing with top insurers like Blue Cross Blue Shield and UnitedHealthcare. Before credentialing, 70% of their clients were out-of-pocket. Afterward, they expanded their patient base, gained referrals, and reduced cancellations.
Key Tip: Always begin credentialing 90–120 days before your planned start date. Delays are common, but early preparation ensures you can start billing as soon as you begin practicing.
👉 Explore more details here → Reach out to insurance credentialing service providers for fast-track enrollment.
Our Mental Health Credentialing Process: Step-by-Step
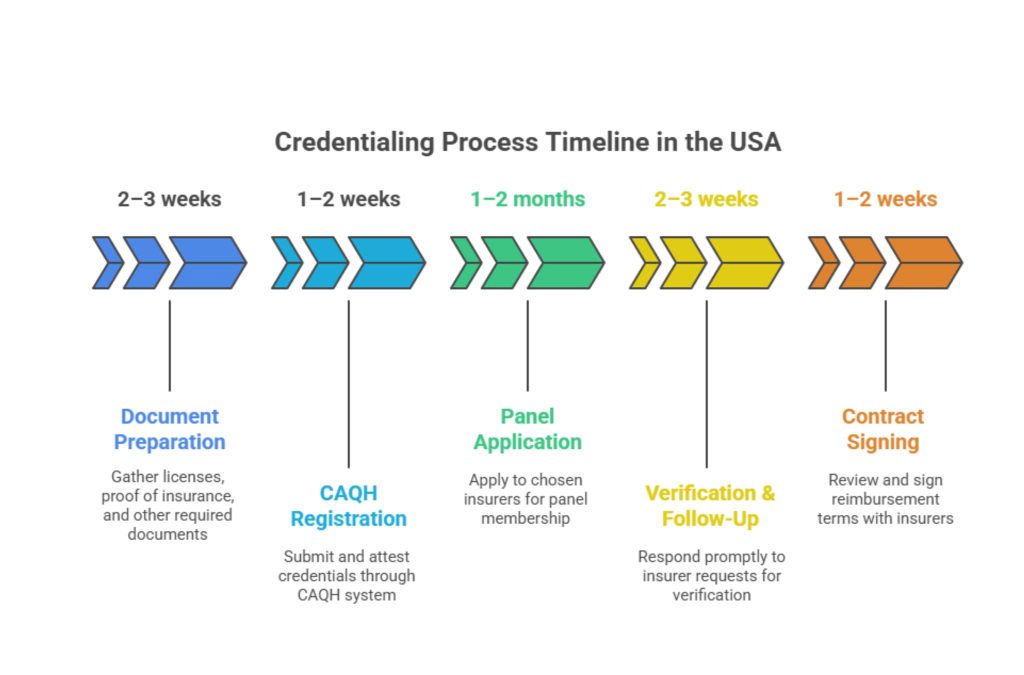
Credentialing may seem overwhelming, but breaking it down into steps makes it manageable. Professional credentialing services follow a structured process that reduces rejection rates and shortens approval timelines.
Step 1: Initial Assessment
Collect and verify provider documents: licenses, degrees, malpractice insurance, work history, and NPI (National Provider Identifier).
Step 2: CAQH Registration
Submit credentials to CAQH ProView, the standard database used by most U.S. insurers. Keep your CAQH profile updated and attested every 120 days.
Step 3: Insurance Panel Applications
Apply to targeted insurance networks like Aetna, Cigna, Humana, or state-specific Medicaid programs. Tailor applications to each insurer’s requirements.
Step 4: Follow-Up and Verification
Insurance companies often request additional details or corrections. Consistent follow-ups reduce processing delays.
Step 5: Contracting and Agreement
Once approved, providers sign contracts that outline reimbursement rates, billing requirements, and compliance obligations.
| Credentialing Step | Timeline (Average) | Key Action |
| Document Preparation | 2–3 weeks | Gather licenses, proof of insurance |
| CAQH Registration | 1–2 weeks | Submit & attest credentials |
| Panel Application | 1–2 months | Apply to chosen insurers |
| Verification & Follow-Up | 2–3 months | Answer insurer requests promptly |
| Contract Signing | 1–2 weeks | Review reimbursement terms |
Result: A streamlined credentialing process reduces approval times from 180 days to as little as 90 days.
👉 Takeaway: Use credentialing service partners to manage follow-ups and negotiate contracts on your behalf.
Mental Health Provider Credentialing Services: Managing CAQH Profiles Across Multiple States
This is a frequent question among therapists expanding across state lines. The answer is no—you do not need multiple CAQH profiles. CAQH ProView is a centralized system, and providers maintain one universal profile. However, you must keep state licenses, addresses, and liability insurance details updated within your profile.
| Scenario | Action Required in CAQH |
| Moving to another state | Update license and practice address |
| Practicing in multiple states | Add all licenses to a single CAQH profile |
| Working in telehealth | Ensure telehealth licenses are linked to your profile |
Expert Insight: Many providers mistakenly create duplicate CAQH accounts, which delays applications. Always use your NPI number to manage a single profile.
👉 Explore more details here → Save time and compliance headaches by keeping your CAQH profile updated every quarter.
Why Credentialing Is Essential for Mental Health Professionals – Maximize ROI and Trust
Credentialing is not just an operational step—it’s an ROI driver. For example, a solo practice in Texas that invested in credentialing saw their patient base grow by 70% within 18 months, with insurance reimbursements forming 80% of their revenue.
Pros:
- Builds patient trust.
- Expands practice reach through insurance networks.
- Provides steady reimbursement revenue.
Cons:
- Time-consuming (90–180 days).
- Complex paperwork and follow-ups.
- Reimbursements vary by insurance company.
| ROI Insight | Impact |
| Credentialed vs. Non-Credentialed Providers | Credentialed see 2–3x client growth |
| Insurance vs. Self-Pay Models | Insurance billing stabilizes revenue, reduces cancellations |
Takeaway: Credentialing transforms a private practice into a sustainable business model, not just a therapeutic service.
👉 Explore more details here → Partner with professional credentialing firms to reduce rejections and speed up ROI.
State-by-State Credentialing Differences for Mental Health Providers Across the USA
Credentialing is regulated at both federal and state levels, meaning requirements differ across regions.
Examples:
- California: Requires specific Medi-Cal enrollment forms alongside commercial applications.
- New York: State Medicaid requires fingerprint-based background checks.
- Texas: Mandates documentation of 3 years of supervised practice for LPCs.
| State | Unique Requirement |
| California | Medi-Cal-specific forms |
| New York | Fingerprint checks |
| Texas | Supervised practice documentation |
| Florida | Telehealth credentialing expansion |
Result: Providers practicing in multiple states must adapt their credentialing strategy to meet regional requirements.
👉 Key Tip: Always check with state boards before starting credentialing to avoid delays.
Key Steps in the Process of Insurance Credentialing for Therapists – Lead Generation & Conversion
Credentialing directly impacts marketing and patient acquisition. Many directories and insurance networks list credentialed providers, improving visibility.
Step-by-Step for Lead Conversion:
- Complete CAQH profile.
- Apply to insurance panels.
- Get listed in insurer directories.
- Optimize profile for SEO and local patient searches.
- Use insurance acceptance in marketing.
| Conversion Strategy | Result |
| Directory Listings | Increases organic patient referrals |
| Insurance Branding | Enhances credibility and SEO |
| Local SEO + Credentialing | Improves Google My Business rankings |
Takeaway: Credentialing is not only about billing—it’s about visibility and conversions.
👉 Explore more details here → Add “Now accepting Aetna, BCBS, Cigna” to your website for immediate patient trust.
Initial Provider Credentialing – Step-by-Step Checklist for Tier One Providers
- Gather licenses, degrees, malpractice insurance.
- Create or update CAQH profile.
- Identify insurance panels (Medicaid, Medicare, commercial).
- Submit applications with supporting documents.
- Track applications and respond quickly to insurer requests.
- Review and sign contracts.
Checklist Result: Following this process reduces rejection rates and ensures compliance.
👉 Takeaway: Keep a digital binder of all updated documents for faster resubmissions.
Commercial Insurance Panel Applications – How to Ensure High Acceptance Rates
To maximize acceptance:
- Apply early and target multiple insurers.
- Ensure your CAQH profile is 100% complete.
- Provide malpractice coverage above minimum limits.
- Highlight specialty areas (child therapy, trauma, couples counseling).
Result: Providers with complete CAQH profiles are 3x more likely to be approved by top commercial panels.
👉 Explore more details here → Outsourcing applications to credentialing services raises acceptance success rates.
SimplePractice’s Powerful EHR – Streamlining Credentialing and Revenue Management
SimplePractice integrates EHR, billing, and credentialing in one platform. Providers can track applications, manage insurance claims, and streamline reimbursement.
Case Study: A solo therapist in Boston reduced claim denials by 35% using SimplePractice’s integrated credentialing and billing tools.
👉 Takeaway: Using EHR platforms with credentialing features saves time and increases reimbursement accuracy.
Search Insights: Top Credentialing Tips for Mental Health Professionals in the USA
- Start credentialing 90–120 days early.
- Keep your CAQH attested quarterly.
- Apply to 4–6 insurers to maximize coverage.
- Use EHR-integrated tools for tracking.
- Consider outsourcing for speed and accuracy.
👉 Explore more details here → Stay proactive; credentialing delays can cost thousands in missed revenue.
Recent Posts: Case Studies and Best Practices for Credentialed Therapists
Example:
- A California practice improved ROI by expanding into Medi-Cal after credentialing.
- An Australian counseling center boosted patient intake by credentialing with private insurers like Medibank.
- A UK therapist doubled referrals after NHS credentialing approval.
👉 Takeaway: Credentialing success stories prove the ROI potential across markets.
Categories: Credentialing, Insurance Panels, and Tier One Market Trends
Credentialing isn’t static—policies evolve. Current trends include:
- Telehealth credentialing growth.
- Automated CAQH updates.
- EHR–credentialing integrations.
- State-specific compliance expansions.
👉 Explore more details here → Stay ahead by monitoring insurance credentialing market shifts.
Types of Insurance Clinicians Typically Consider – Key Insights & ROI Stats
- Commercial Insurance (Aetna, BCBS, Cigna): Broadest reach, moderate reimbursement.
- Medicare/Medicaid: Essential for older adults and low-income clients.
- Private Insurers in UK, Canada, Australia: Key for Tier One international practices.
ROI Insight: Practices credentialed with both commercial and government panels report 2.5x higher revenue stability.
👉 Takeaway: Diversify panels to minimize risk and maximize ROI.
Traditional Medicare Credentialing – Step-by-Step Guidance for Mental Health Providers
Medicare requires:
- NPI registration.
- PECOS enrollment (Provider Enrollment, Chain, and Ownership System).
- Approval from CMS (Centers for Medicare & Medicaid Services).
Result: Once approved, providers can serve Medicare clients, a rapidly growing population in the U.S.
👉 Explore more details here → Medicare credentialing expands long-term patient sustainability.
FAQs
1. What are the best credentialing services for mental health providers in the USA, UK, Canada, and Australia?
The best services include SimplePractice, Ensora Health, and AdvancedMD in the USA, along with NHS-approved credentialing pathways in the UK, Medibank credentialing platforms in Australia, and provincial insurer programs in Canada. These services simplify applications, maintain compliance, and provide automated follow-ups. A provider in Toronto, for example, saw faster approvals by using provincial digital credentialing tools. Key takeaway: choose platforms that align with local insurance frameworks for the highest efficiency and ROI.
2. How much does it cost to get credentialed with insurance companies as a therapist in 2025?
Costs vary between $2,000–$4,000 for full-service credentialing agencies in the USA, while UK and Australian providers typically pay £1,500–£2,500 or AUD 3,000–5,000. DIY credentialing may cost less but consumes hundreds of hours of admin time. Hidden costs include malpractice insurance upgrades and license renewals. Key tip: investing in professional services pays off—approved providers often recover costs within the first 3–6 months of insurance reimbursements.
3. Which credentialing process offers the highest ROI and fastest insurance acceptance for mental health professionals?
Using a hybrid model—professional credentialing services plus EHR integration—offers the best ROI. Agencies manage paperwork and follow-ups, while EHR platforms automate claims. This reduces rejections and speeds approval. Case study: A New York practice credentialed with four insurers within 120 days, cutting average approval time by 40% and doubling revenue in under a year. The combination of outsourcing and digital automation consistently provides the fastest and most cost-effective path.
4. How do I maintain multiple CAQH profiles if practicing in multiple states?
You don’t need multiple profiles. A single CAQH profile can cover all licenses across different states. Simply update your profile with each new state license, practice address, and liability coverage. Maintaining one account avoids duplication errors and ensures insurers have consistent data. Pro tip: set quarterly reminders to update and attest your CAQH to prevent credentialing delays across multiple states.
5. What are the top insurance panels and credentialing requirements for clinical mental health providers?
The most sought-after panels in the U.S. include Aetna, Blue Cross Blue Shield, Cigna, Humana, and UnitedHealthcare. Requirements include a valid state license, malpractice insurance, updated CAQH, and proof of education. In the UK, NHS panels remain dominant, while Australia prioritizes Medibank and Bupa. Canada’s system varies by province but includes regional insurers like Sun Life and Manulife. Providers should aim to join at least 4–6 major panels to balance reach and revenue.
6. How can credentialing improve lead generation and client conversion for private practices?
Credentialed providers appear in insurance directories, which patients actively use to find therapists. Being listed on platforms like Aetna’s provider directory or NHS Directories boosts visibility. Patients are more likely to choose covered providers, reducing out-of-pocket costs. This increases referrals, improves conversion rates, and stabilizes revenue streams. Adding insurance logos to websites and marketing materials further enhances credibility and client acquisition.
7. Checklist: Step-by-step credentialing for therapists and counselors in Tier One countries.
- Verify licenses and certifications.
- Prepare malpractice insurance proof.
- Create or update CAQH profile (USA).
- Apply to national or regional insurance panels.
- Respond to follow-up requests promptly.
- Review and sign contracts.
In Canada and Australia, use regional insurer systems, while in the UK, work through NHS credentialing channels. Following this checklist ensures smooth enrollment and fewer rejections.
8. Comparison: SimplePractice vs AdvancedMD vs Ensora Health for insurance credentialing and management.
- SimplePractice: Best for solo providers, integrates EHR and billing.
- AdvancedMD: Ideal for mid-size practices, offers deep reporting tools.
- Ensora Health: Focused on enterprise-level practices, optimized for high-volume credentialing.
Case study: A Boston practice used SimplePractice to cut claim denials by 30%, while a Texas clinic leveraged AdvancedMD to scale group practice billing. Each option serves a different tier, but all improve credentialing speed and ROI.
9. What are the industry trends and best practices for mental health provider credentialing in the USA & UK?
Trends include telehealth credentialing expansion, digital CAQH updates, and EHR integrations. Best practices involve maintaining updated profiles, applying to multiple panels, and outsourcing follow-ups. In the UK, NHS credentialing is moving toward streamlined digital systems, while U.S. insurers are adopting AI-driven verification tools. Practices adopting these trends report 20–30% faster approvals and stronger compliance.
10. How long does it take to complete credentialing and start billing insurance companies effectively?
On average, credentialing takes 90–180 days. Solo providers may take longer due to follow-up delays, while agencies can expedite approvals. Billing typically starts within 30 days of contract signing. Key takeaway: start early—apply 3–6 months before practice launch or expansion to avoid revenue gaps. Once credentialed, providers can begin billing insurers immediately, creating stable revenue flow.
