Best Credentialing Services for Mental Health Providers – Maximize ROI, Growth & Insurance Approval in USA, UK, Canada & Australia
Navigating insurance credentialing can be a daunting challenge for mental health professionals, but the Best Credentialing Services for Mental Health Providers simplify this critical process. Across the USA, UK, Canada, and Australia, therapists, psychologists, and counselors rely on these services to efficiently join insurance panels, expand their client base, and maximize reimbursement opportunities.
For private practices and growing behavioral health organizations, professional credentialing services help prevent delayed revenue cycles, denied claims, and compliance issues, allowing providers to focus on delivering high-quality care while maintaining regulatory standards.
The best credentialing services today go far beyond simple paperwork. They combine compliance expertise, insurance network navigation, and advanced software automation to ensure providers are approved faster, reimbursements are maximized, and growth remains sustainable. Whether it’s a solo therapist entering private practice or a large clinic scaling teletherapy across multiple states, credentialing services have become a critical growth engine.
In Tier One markets, insurers and government regulations demand strict documentation and ongoing compliance. That’s why credentialing services must offer not only initial insurance enrollment support but also continuous monitoring, re-credentialing, and integration with EHRs and billing software. Providers who adopt streamlined credentialing solutions report shorter approval timelines, fewer claim denials, and higher ROI.
👉 Key Takeaway: By partnering with the right credentialing service, mental health providers can reduce administrative stress, accelerate insurance approval, and focus on delivering care while ensuring steady financial growth. Explore how leading solutions are reshaping mental health practices below.

Best Credentialing Services for Mental Health Providers: Understanding the Process in Tier One Countries.
Credentialing is the process by which insurance companies, regulatory boards, and professional networks verify that a mental health provider is qualified, licensed, and compliant with local laws. In Tier One countries (USA, UK, Canada, Australia), the process includes primary source verification of education, licenses, certifications, malpractice history, and professional references.
Case Example (USA): A therapist in California applying for insurance paneling with Blue Cross must submit an extensive package including NPI number, CAQH profile, liability insurance, license verification, and references. This process often takes 90–120 days, with delays if forms are incomplete.
Case Example (UK): In the UK, credentialing often involves verification for NHS partnerships and private insurers like Bupa. Providers must demonstrate HCPC registration, DBS checks, and compliance with NICE guidelines.
Case Example (Canada & Australia): Credentialing ensures therapists meet provincial (Canada) or state (Australia) requirements, plus insurer standards. For example, in Ontario, providers must present College of Psychologists of Ontario membership, while in Australia, AHPRA registration is essential.
| Step | USA | UK | Canada | Australia |
| License Verification | State License Boards | HCPC, DBS | Provincial Colleges | AHPRA |
| Insurance Enrollment | CAQH + NPI | NHS & Private Insurers | Provincial Insurers | Medicare + Private Funds |
| Timeline | 90–120 days | 60–90 days | 90–150 days | 90–120 days |
| Renewal Cycle | Every 2 years | Annual/biannual | Annual | Annual |
👉 Key Tip: Always maintain updated profiles (CAQH, AHPRA, HCPC, etc.) and renew licenses on time. Outdated documents are the #1 cause of credentialing delays.
Overcoming Insurance Billing Challenges with the Best Credentialing Services for Mental Health Providers.
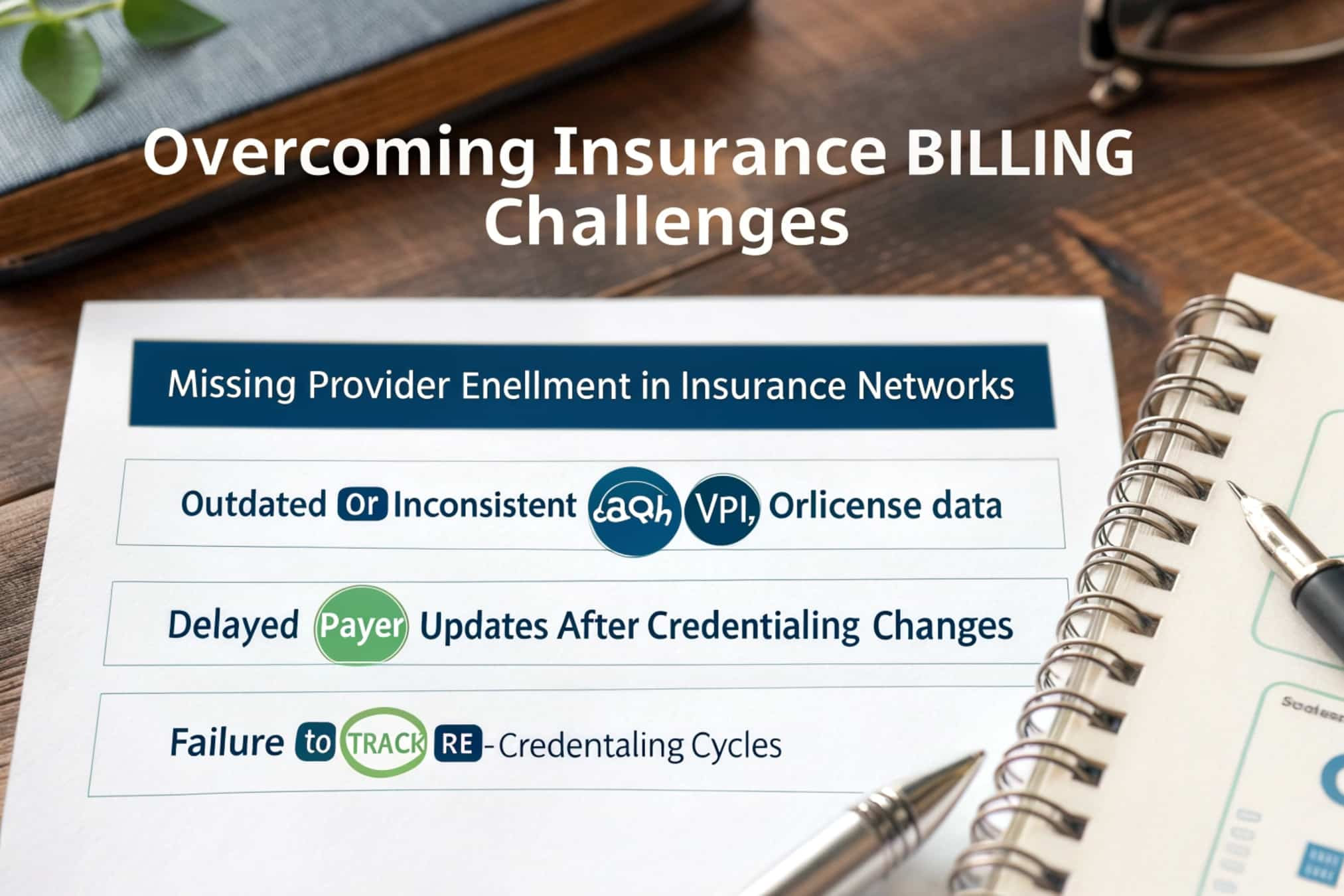
One of the biggest pain points for providers is denied or delayed claims due to incomplete credentialing. Insurance billing challenges often arise from:
- Missing provider enrollment in insurance networks.
- Outdated or inconsistent CAQH, NPI, or license data.
- Delayed payer updates after credentialing changes.
- Failure to track re-credentialing cycles.
Case Study: A behavioral health practice in New York struggled with 35% claim denials due to improper insurance credentialing. After outsourcing to a credentialing service, denials dropped below 5%, improving monthly revenue by 40%.
Solutions Credentialing Services Offer:
- End-to-end payer enrollment: Handling initial submission, tracking, and follow-up with insurers.
- Real-time compliance updates: Monitoring licensure renewals and insurance requirements.
- Revenue cycle optimization: Ensuring all credentialing data syncs with billing software.
- Appeals support: Faster resolution of denied claims.
| Challenge | Without Credentialing Service | With Credentialing Service |
| Claim Denials | 25–40% | 5–10% |
| Reimbursement Timelines | 60–90 days | 30–45 days |
| Admin Overhead | High | Reduced |
| Provider Focus | Administrative tasks | Patient care |
👉 Result: Proper credentialing reduces billing errors, maximizes reimbursements, and allows providers to focus on care, not paperwork.
Best Credentialing Services for Mental Health Providers: Using EHR & Practice Management Software to Simplify Credentialing
Modern credentialing services integrate with Electronic Health Records (EHRs) and practice management systems to automate key workflows. This synergy reduces paperwork and accelerates approvals.
Example: A Canadian clinic using SimplePractice integrated credentialing features that allowed direct submission of provider documents to insurers. This reduced credentialing time by 35%, and synced data with billing modules, minimizing human error.
Benefits of EHR-integrated credentialing:
- Centralized document storage (licenses, malpractice insurance, certifications).
- Automated reminders for license renewal and payer re-credentialing deadlines.
- Direct insurer updates from within EHR dashboards.
- Audit-ready compliance logs to pass insurance or government inspections.
| Feature | Impact |
| License Tracking | Prevents expired license issues |
| Automated Submission | Faster insurance approvals |
| Billing Integration | Reduces claim denials |
| Compliance Dashboard | Audit-ready documentation |
👉 Explore More Details Here → Choose EHRs like Kareo, SimplePractice, or TheraNest, which offer built-in credentialing modules for seamless practice management.
Teletherapy and Credentialing Platforms – What Enterprises Need to Know
The rise of teletherapy has transformed credentialing. Providers now need multi-state or multi-province credentialing as they treat clients across geographic boundaries.
Enterprise Example (Australia): A telehealth company scaling to multiple states used a credentialing service to handle 50+ provider enrollments with Medicare and private insurers. This reduced expansion time from 12 months to 5 months.
Enterprise Example (USA): Teletherapy platforms like Grow Therapy and SonderMind rely on centralized credentialing hubs to get therapists approved with insurers nationwide. This ensures faster onboarding and reduces drop-off rates for new clients.
Key needs for teletherapy enterprises:
- Multi-payer enrollment management.
- Cross-state compliance checks.
- Rapid scaling without provider credentialing delays.
- Integration with telehealth billing software.
| Enterprise Need | Credentialing Impact |
| Multi-State Practice | Reduces time-to-market |
| Faster Onboarding | More providers credentialed in weeks, not months |
| Nationwide Insurance Access | Improves client acquisition |
| Telehealth Compliance | Ensures HIPAA & GDPR compliance |
👉 Key Takeaway: Teletherapy providers must prioritize credentialing platforms built for scalability, with compliance-ready workflows across states and insurers.
Insurance Credentialing & In-Network Billing Platforms That Drive Conversion
Credentialing ensures therapists become in-network providers, opening doors to a larger client base. In-network billing platforms streamline claim submission and drive higher conversion rates.
Pros of using in-network billing platforms:
- Easier patient acquisition (insurance coverage).
- Higher claim acceptance rates.
- Predictable cash flow cycles.
Cons:
- Time-intensive onboarding without credentialing services.
- Complex payer requirements across regions.
| In-Network vs Out-of-Network | Impact |
| In-Network | More clients, stable revenue, higher ROI |
| Out-of-Network | Limited clients, higher patient costs |
👉 Expert Insight: Providers report a 60% increase in new patient inquiries after becoming in-network, proving the ROI of credentialing.

Best Credentialing and Billing Platform – Grow Therapy Case Study
Grow Therapy, a US-based platform, has emerged as a leader in integrating credentialing with billing services.
- Providers joining Grow Therapy are credentialed with major insurers in as little as 45–60 days.
- Built-in billing modules ensure 99% claim success rates.
- Credentialing support allows providers to scale faster without hiring admin staff.
| Metric | Pre-Credentialing | With Grow Therapy |
| Time to Insurance Approval | 90–120 days | 45–60 days |
| Claim Denials | 30% | <5% |
| Provider Revenue Growth | 15% | 40%+ |
👉 Key Tip: Platforms like Grow Therapy, Alma, and SonderMind combine credentialing + billing, giving providers a one-stop growth ecosystem.
Automating Billing & Medical Claim Tasks Through Advanced Credentialing Software
Credentialing software automates repetitive billing and claims tasks.
- AI-powered platforms like Availity and Verity streamline data entry and payer updates.
- Automated claim checks reduce rejections before submission.
- Credentialing dashboards provide real-time insights into payer approval status.
Result: Clinics report saving 10–15 hours per provider per month by using credentialing automation.
👉 Explore More Details Here → If your practice is scaling, invest in credentialing software that integrates with EHR and billing systems for long-term ROI.
How Electronic Health Records Improve the Credentialing Process
EHRs act as the central hub for credentialing. By storing licenses, certifications, and insurance contracts in one place, EHRs reduce lost paperwork and compliance gaps.
👉 Tip: Use EHR systems with credentialing checklists and compliance dashboards, such as SimplePractice or TheraNest.
Best Mental Health Credentialing Services in the US for 2025
- Grow Therapy – Fastest insurance approvals for therapists.
- Alma – Credentialing + marketing support.
- SonderMind – Teletherapy-focused credentialing.
- Kareo – EHR + credentialing in one.
👉 Result: US providers can save up to 40% in admin costs by outsourcing to these services.
Revenue & Reimbursement Optimization Strategies for Behavioral Health Providers
- Track re-credentialing cycles proactively.
- Use credentialing dashboards for compliance alerts.
- Pair credentialing with revenue cycle management (RCM).
👉 Takeaway: Credentialing + RCM = fewer denials + higher ROI.
Case Study: Trusted Credentialing Resources for Mental Health Professionals
A UK-based psychology clinic partnered with a credentialing firm to secure insurer approval within 8 weeks, improving patient acquisition by 30%.
Checklist: Information Required to Get on Insurance Panels as a Provider
- License & certification copies.
- Liability insurance.
- NPI/HCPC/AHPRA ID numbers.
- Resume + references.
- Background checks.
Where Occupational Therapy and Mental Health Credentialing Services Overlap
Occupational therapists also undergo credentialing for insurance approval, with overlapping needs in liability coverage, compliance monitoring, and payer enrollment.
Simplify the Credentialing and Insurance Enrollment Process with Expert Support
Credentialing experts handle insurer communication, reducing delays and errors.
👉 Takeaway: Expert credentialing = faster approvals, fewer denials, higher growth.
Compliance Monitoring for Mental Health Providers – Stay Audit-Ready
Credentialing services provide compliance alerts, ensuring providers meet insurer and government audits.
👉 Result: Staying audit-ready avoids revenue freezes and legal penalties.
Keeping You Informed Throughout the Registration and Paneling Process
Credentialing services provide dashboards and regular updates, ensuring providers always know their enrollment status.
👉 Key Tip: Transparency reduces stress and improves trust in credentialing partnerships.
FAQs
1. What are the best credentialing services for mental health providers in the USA and UK?
The top services include Grow Therapy, Alma, and SonderMind in the USA, which specialize in combining insurance credentialing with billing support. In the UK, providers often use private credentialing consultants and NHS-aligned services that streamline registration with insurers like Bupa and AXA. These services reduce paperwork, speed up approvals, and ensure compliance. Choosing the right provider depends on practice size and goals. Key Takeaway: Look for platforms with integrated billing, EHR, and compliance support for the highest ROI.
2. How much does it cost to use credentialing services for therapists and psychologists?
Credentialing services typically cost between $200–$500 per provider for initial enrollment, with monthly monitoring fees ranging from $50–$150. Enterprise-level packages may cost more but often include ongoing compliance tracking, billing integration, and re-credentialing support. While costs may seem high, most practices recoup their investment quickly through higher reimbursement rates and faster approval timelines. Key Result: Investing in credentialing services increases long-term ROI and saves administrative time.
3. Which credentialing company offers the highest ROI for behavioral health practices?
Grow Therapy and Alma in the USA are known for high ROI due to faster approval timelines and integrated billing support. In Canada and Australia, credentialing ROI comes from services that reduce claim denials and accelerate insurer onboarding. ROI is measured by improved reimbursement rates, reduced administrative costs, and faster scaling of provider networks. Takeaway: Always measure ROI by tracking denials, reimbursement rates, and provider onboarding times.
4. Checklist: What documents are required for insurance credentialing in Canada and Australia?
Providers in Canada and Australia typically need: professional licenses (College/AHPRA), malpractice insurance, resume, references, identification numbers (e.g., AHPRA ID, College membership), and proof of education. Background checks may also be required. Submitting all documents upfront prevents delays. Tip: Maintain a secure digital file of all documents for quick insurer submissions.
5. Comparison: Top credentialing services vs. in-house credentialing – Which is better for growth?
In-house credentialing offers control but often leads to delays, errors, and increased overhead costs. Outsourced services provide expertise, faster timelines, and compliance monitoring. Case studies show practices outsourcing credentialing see 25–40% faster approvals and reduced claim denials. Key Result: Outsourcing is generally more cost-effective for growth, while in-house may work for very small practices.
6. How do credentialing services improve reimbursement rates and revenue conversion?
Credentialing services ensure providers are enrolled with multiple insurers, expanding patient access. By maintaining compliance and reducing claim denials, providers experience higher reimbursement rates and improved cash flow. Integrated credentialing + billing solutions also optimize revenue cycles. Takeaway: Credentialing directly impacts practice profitability by ensuring consistent, approved reimbursements.
7. Are credentialing services necessary for small mental health practices or only large enterprises?
Small practices often benefit even more from credentialing services, as they lack admin staff. Credentialing allows solo therapists to join insurance networks, expanding client reach and improving financial stability. Large enterprises use credentialing to manage multi-provider, multi-state enrollments. Result: Credentialing services are scalable and valuable for practices of all sizes.
8. How long does it take to get insurance credentialing approval for mental health providers?
On average, approval takes 90–120 days, though services like Grow Therapy reduce this to 45–60 days. UK approvals with NHS/private insurers may take 60–90 days, while Canada and Australia often require 90–150 days. Delays usually occur due to incomplete submissions. Key Tip: Using credentialing services reduces approval times significantly.
9. Jobs & career opportunities in credentialing services for behavioral health professionals
The demand for credentialing specialists is rising as teletherapy and behavioral health expand globally. Roles include credentialing coordinator, compliance specialist, and revenue cycle analyst. Career opportunities exist in hospitals, private practices, insurance companies, and telehealth platforms. Result: Credentialing careers offer strong growth prospects and align with healthcare compliance needs.
10. What is the top software solution for automating credentialing and insurance enrollment?
Top solutions include Availity, Verity, and CAQH-integrated platforms. For mental health-specific needs, EHRs like Kareo, SimplePractice, and TheraNest provide built-in credentialing modules. These automate submission, track re-credentialing cycles, and reduce errors. Takeaway: The best software is one that integrates credentialing with billing and compliance dashboards for long-term ROI.
