Best Companies for Mental Health Billing in 2025 – Maximize Revenue & ROI for USA, UK, Canada & Australia
Mental health billing is one of the most challenging parts of running a behavioral health practice. Therapists, psychologists, psychiatrists, and large behavioral health enterprises often spend more hours on coding, claim denials, and compliance than on client care.
With the introduction of new 2025 compliance updates in the USA, UK, Canada, and Australia, mental health billing complexities have become even more demanding. That’s why partnering with the best companies for mental health billing in 2025 can completely transform your revenue cycle and reduce administrative stress.
In Tier One markets, mental health billing companies now combine advanced automation, AI-driven denial management, and expert human oversight to increase approval rates, optimize insurance reimbursements, and ensure practices remain fully compliant. The best companies for mental health billing don’t just process claims—they help you grow, scale, and improve patient experience by minimizing operational burdens.
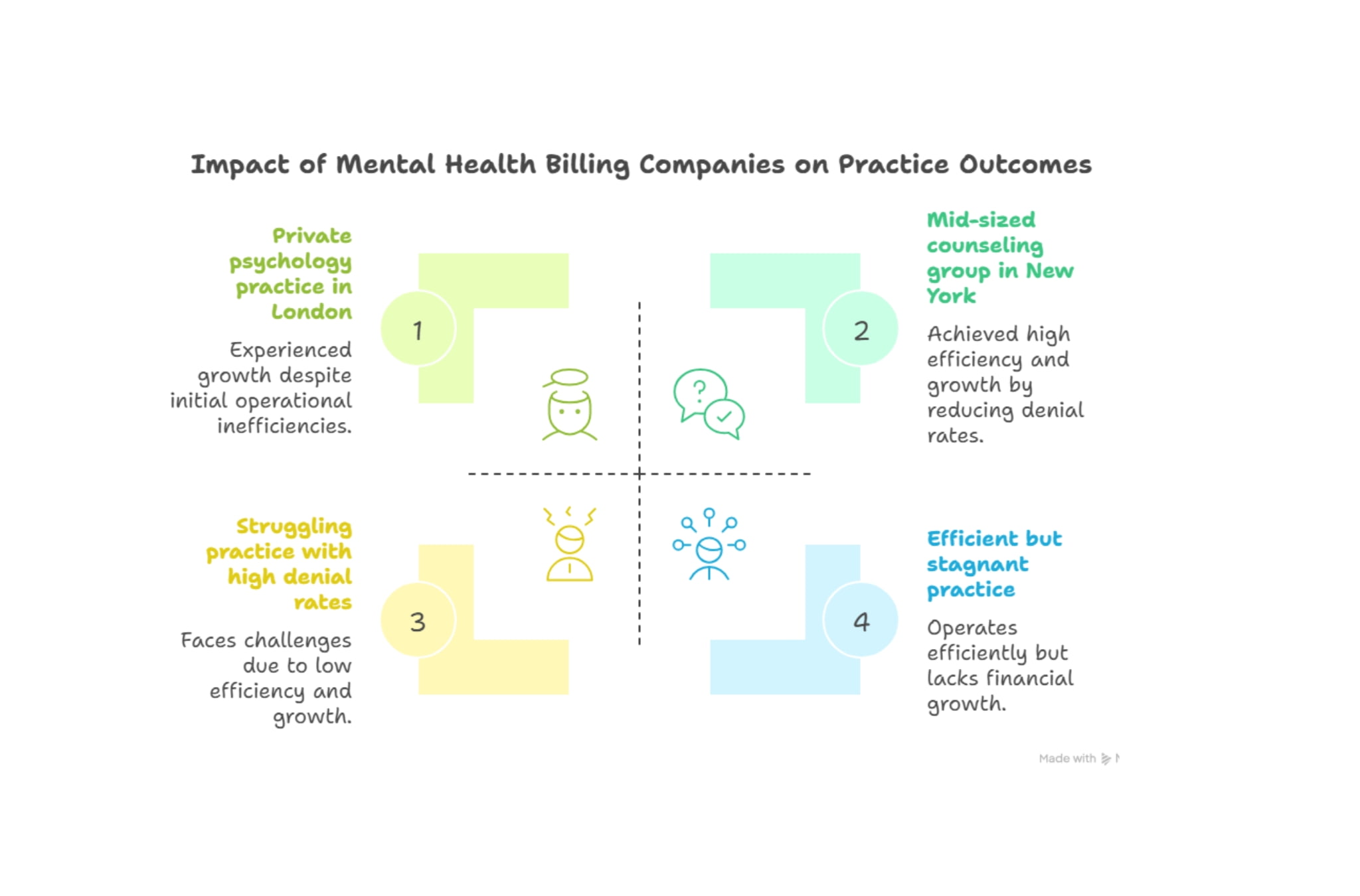
Consider the case of a mid-sized counseling group in New York: after outsourcing to one of the best mental health billing companies, their denial rate dropped from 18% to 5% within six months. Similarly, a private psychology practice in London doubled its cash flow by switching to a company that specialized in behavioral health insurance billing. These success stories highlight a key fact: choosing the right billing partner has a direct impact on ROI, growth, and peace of mind.
If you’re searching for the best companies for mental health billing in 2025, this guide provides a comprehensive breakdown—covering key challenges, solutions, services, compliance updates, and expert tips—to help you maximize revenue while keeping your focus where it belongs: client care.
Mental Health Billing

“Best Companies for Mental Health Billing in 2025: Keys to Overcoming Mental and Behavioral Health Billing Challenges for Enterprises”
Behavioral health billing is notoriously complex. Unlike general medical billing, it involves unique codes (e.g., 90791 for psychiatric diagnostic evaluations, 90834 for psychotherapy), frequent use of modifiers, and varying rules across insurers. These complexities make it challenging for practices to manage billing efficiently, especially as new 2025 regulations come into effect.
Many organizations now rely on the best companies for mental health billing in 2025 to handle coding accuracy, payer requirements, and evolving compliance standards. Enterprises managing hundreds of providers often face three major obstacles: claim denials, credentialing delays, and slow reimbursements—issues that top mental health billing companies are equipped to solve through automation, expert oversight, and proven workflows.
Case Study – Australia: A large behavioral health clinic in Sydney faced 30% claim denials due to coding errors. After adopting specialized billing software and outsourcing to a company with psychiatric coding experts, their denial rate dropped below 7%, unlocking nearly $250,000 in lost annual revenue.
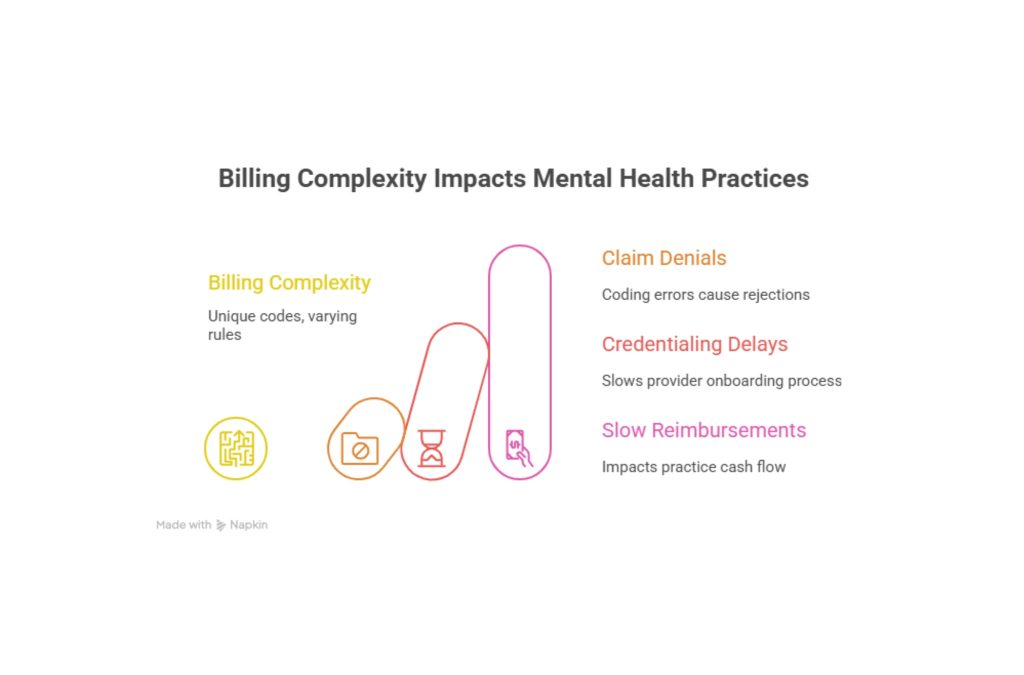
Table – Key Billing Challenges vs. Solutions
| High denial rates | Lost revenue & admin burden | AI-driven denial management & coding accuracy |
| Credentialing delays | Delayed reimbursements | Dedicated credentialing teams |
| Compliance updates | Risk of penalties | Real-time compliance monitoring |
| Transparency gaps | Poor financial oversight | Custom financial reporting dashboards |
Key Takeaway: Effective mental health billing requires a powerful combination of automation and specialized human expertise. To stay ahead of complex regulations and evolving payer rules, enterprises in the US, UK, Canada, and Australia should partner with the best companies for mental health billing in 2025. These companies focus on compliance-first strategies, transparent reporting, and 24/7 denial management to ensure smooth operations. By working with top mental health billing companies, behavioral health practices can minimize errors, reduce claim denials, and maximize insurance reimbursements efficiently.
Explore more details here → Trusted partners, such as NCDS, Kareo, and AdvancedMD, now offer dedicated behavioral health billing divisions to address these enterprise-level challenges.
Best EHR for Mental Health Private Practice–https://healthnagari.com/2025/10/01/best-ehr-for-mental-health-private-practice/#more-372
Registration Open: 2025 Behavioral Health Billing Solutions Annual 2-Day Seminar
In February 2025, the Annual Behavioral Health Billing Solutions Seminar will bring together experts from the USA, UK, Canada, and Australia to share strategies for reducing denials, streamlining credentialing, and improving cash flow.
Highlights include:
- Day 1: Deep dive into compliance updates (HIPAA, NHS guidelines, Canadian PIPEDA, and Australia’s Medicare changes).
- Day 2: Case studies from billing companies demonstrating ROI growth for both small practices and enterprises.
Single
Enrich our growing community.
- General admission and member discounts for one adult
- One free ticket per special exhibition
- Two single-use guest passes per year
Family
Support special exhibitions.
- General admission and member discounts for two adults
- Four free tickets per special exhibition
- Four single-use guest passes per year
Patron
Take support to the next level.
- General admission and member discounts for two adults
- Five free tickets per special exhibition
- Six single-use guest passes per year
Table of Contents
Mini Case Study – UK: A psychiatrist group in Manchester partnered with a top billing provider after attending the 2024 seminar. Within three months, they increased approval rates by 40% and secured faster reimbursements.
Table – Seminar Benefits
| Live coding workshops | Therapists & psychologists |
| Compliance updates | Administrators & directors |
| Technology showcases | Enterprises & hospitals |
| Networking | Providers & billing specialists |
Key Tip: Attending seminars not only updates providers on billing changes but also connects them with potential billing partners, saving months of trial and error.
Explore more details here → Register now to secure early-bird discounts and get exclusive access to billing company evaluation checklists.
Important Updates for Behavioral Health Providers – February 2025 Compliance & Growth
2025 brings critical compliance updates for behavioral health billing, making it more important than ever to partner with the best companies for mental health billing in 2025. In the USA, providers must now adhere to updated HIPAA interoperability rules, ensuring secure and efficient data exchange. The UK is rolling out enhanced NHS claim review standards, while Canada has revised reimbursement timelines under its provincial healthcare plans. Meanwhile, Australia has updated telehealth billing regulations under Medicare. Leading mental health billing companies are adapting rapidly to these changes, helping behavioral health practices maintain compliance, avoid costly denials, and keep revenue cycles running smoothly.
Case Study – Canada: A Toronto-based mental health clinic lost 15% of potential revenue due to outdated compliance systems. After switching to a cloud-based billing service, they achieved real-time compliance monitoring and improved revenue cycle speed by 28%.
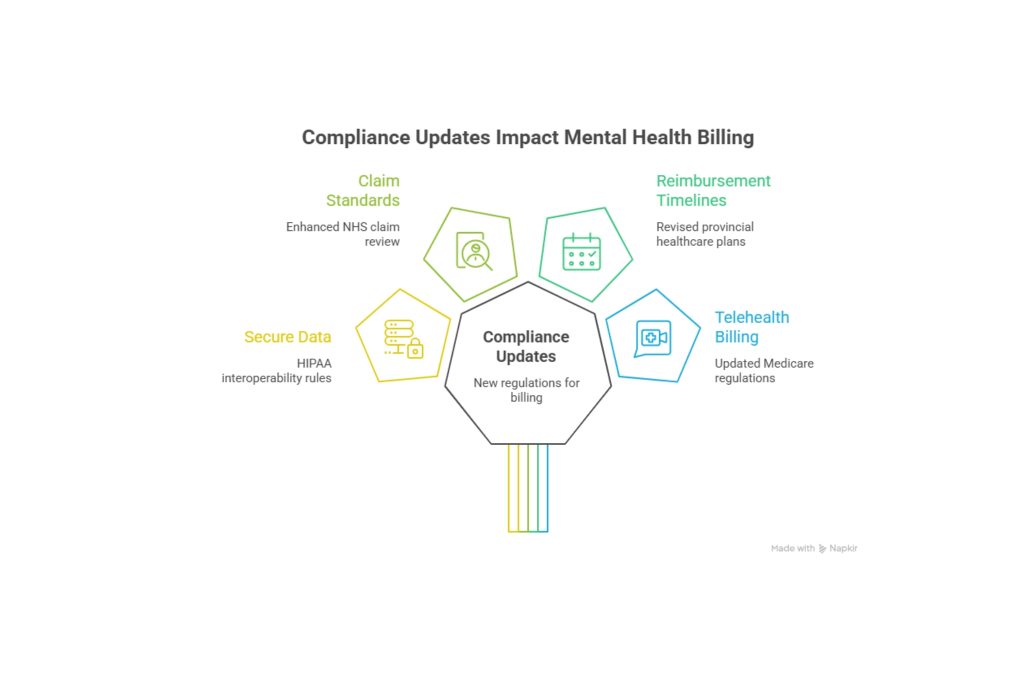
Table – 2025 Compliance Highlights
| USA | HIPAA interoperability rules | Stricter claim data sharing |
| UK | NHS claim review | More audits, higher rejection risk |
| Canada | Provincial reimbursement rules | Faster timelines, but tighter coding |
| Australia | Telehealth under Medicare | Expanded codes, stricter documentation |
Result: Providers who partner with companies that stay ahead of compliance changes experience fewer denials, higher ROI, and reduced legal risks.
Explore more details here → Look for billing companies that publish compliance update bulletins every quarter.
Clients trust practices that are financially transparent and hassle-free. Mental health insurance billing services not only ensure correct claim submissions but also enhance patient trust by reducing surprise bills.
American Medical Billing Association (AMBA):https://www.ambanet.net/
USA HIPAA rules: https://www.hhs.gov/hipaa/index.html
UK NHS: https://www.nhs.uk/
Canada PIPEDA: https://www.priv.gc.ca/en/privacy-topics/health-genetic-and-other-body-information/
Pros & Cons of Outsourcing Mental Health Billing
| Faster reimbursements | Requires vendor selection time |
| Lower denial rates | Monthly service fees |
| Compliance handled by experts | Reliance on third-party |
| Focus more on patient care | Training needed for staff |
Expert Insight: According to the American Medical Billing Association (AMBA), practices that outsourced mental health billing in 2024 saw an average 23% increase in collections.
Key Tip: Showcase billing transparency on your website. Clients are more likely to book therapy sessions if they trust your billing process.
Expert Billing Specialists & Dedicated Industry Professionals for Tier One Providers
The best companies in the US, UK, Canada, and Australia don’t just provide software—they provide people. Dedicated billing specialists know insurer quirks, understand mental health coding, and often act as extensions of your team.
Case Study – USA: A behavioral health enterprise in Los Angeles reduced claim rejections by 60% by assigning a dedicated billing team that handled coding, compliance, and follow-up calls.
Table – Dedicated Billing vs. Generic Billing Services
| Knowledge of behavioral codes | Deep expertise | Limited |
| Denial management | Active follow-up | Reactive only |
| ROI growth | 20–40% increase | Minimal impact |
Result: Practices with dedicated billing specialists report faster ROI and higher patient satisfaction.
Leave the Mental and Behavioral Health Billing to NCDS – Trusted Enterprise Partner
NCDS (National Credentialing & Data Solutions) is among the top trusted partners for behavioral health enterprises. They specialize in credentialing, denial management, and enterprise-level billing across the USA, UK, and expanding markets in Canada and Australia.
Mini Case Study: A London-based psychiatry group partnered with NCDS for credentialing with private insurers. Within six months, their approval timeline dropped from 9 months to 3 months, unlocking faster revenue streams.
Key Takeaway: For companies seeking enterprise-level support with global compliance expertise, NCDS remains a strong choice in 2025.
Step-by-Step Evaluation of Your Client’s Billing Process and Personnel for ROI Growth
Billing companies now offer ROI-focused audits. They evaluate your staff’s coding skills, claim submission process, and denial handling strategies.
Checklist for Evaluation:
- Are codes being used correctly for psychotherapy and group sessions?
- Are denials tracked with root-cause analysis?
- Is there a feedback loop between billing staff and providers?
Micro-CTA: Book a free audit with your billing company to see hidden revenue leaks.
Metrics Reporting That Improves Financial Transparency for Mental Health Providers
Financial transparency builds trust with both patients and investors. Billing companies offer custom dashboards that provide insights into revenue per provider, denial trends, and reimbursement timelines.
Key Tip: Set monthly revenue benchmarks and track them via automated reports for sustainable growth.
Insurance Reimbursement Rates – A Quick Guide for Therapists & Enterprises
Insurance reimbursement rates vary by code, country, and insurer.
Sample Table – Reimbursement Averages (USA)
| 90791 | Psychiatric evaluation | $180–$220 |
| 90834 | Psychotherapy, 45 min | $100–$150 |
| 90837 | Psychotherapy, 60 min | $130–$180 |
Takeaway: Compare rates across insurers annually to negotiate better contracts.
How to Get Credentialed with Insurance Companies for Your Mental Health Practice in the USA & UK
Credentialing remains one of the longest processes in mental health billing. In the USA, it may take 90–120 days; in the UK, NHS and private insurers require strict document submission.
Key Tip: Outsourcing credentialing saves 3–6 months of delays.
Medicaid Billing Rules Explained: How Often Can Code 90785 Be Used by Providers?
Code 90785 (interactive complexity) can only be billed when specific criteria (language barriers, emotional intensity) are met. Medicaid limits its frequency to avoid misuse.
Key Tip: Use documentation templates to justify usage and reduce audit risk.
Ready to Optimize Your Revenue with Our Medical Billing & Coding Experts in Canada & Australia?
Providers in Canada and Australia face unique billing challenges under provincial and Medicare systems. Partnering with coding experts ensures consistent revenue cycles.
Key Tip: Always align billing codes with payer rules to avoid lengthy delays.
Comprehensive Medical Billing Services for Mental Health Professionals – Enterprise Insights
From credentialing and coding to denial management and compliance, comprehensive billing services cover every step.
Result: Enterprises that outsource billing save 25–35% in annual administrative costs.
Spend More Time with Clients, Earn More, and Reduce Stress with Smart Billing Software
Smart billing software integrates with EHRs, automates claim submission, and reduces manual work.
Takeaway: Every hour saved on billing is an hour gained for client care.
Denial Management Strategies That Improve Approval Rates & Cash Flow by 40%
Top billing companies use predictive analytics to flag high-risk claims before submission.
Key Tip: Holding weekly denial review meetings can dramatically reduce rejection rates.
FAQ
1. What are the best billing companies for mental health professionals in the USA and UK?
The best companies for mental health billing in 2025 include trusted providers like NCDS, Kareo, AdvancedMD, and TherapyNotes Billing. In the USA, these firms specialize in HIPAA compliance, multi-state credentialing, and advanced denial management. In the UK, providers such as Priory Billing Services and NHS-compliant third parties dominate the behavioral health billing space, offering seamless claims processing and adherence to national standards. These mental health billing companies are known for lowering denials, expediting reimbursements, and improving revenue transparency. Practices that choose these top billing partners consistently report higher ROI, faster claim turnaround times, and greater efficiency in revenue cycle management.
2. How much does outsourcing mental health billing services cost in 2025?
Outsourcing costs typically range from 4% to 9% of collected revenue. For small practices, fees may start as low as $800/month, while enterprises can expect customized pricing tied to claim volume. Though it’s an upfront expense, outsourcing consistently delivers higher ROI by reducing denials and freeing providers to see more clients. Practices often recover 15%–30% of previously lost revenue, making it a growth investment rather than just a cost of doing business.
3. Which billing company provides the highest ROI for therapists and behavioral health clinics?
NCDS and Kareo lead in ROI due to their dedicated denial management systems and transparent reporting. Clinics using these services see ROI increases of 25%–40% within the first year. ROI depends on claim volume, payer mix, and denial rates; however, billing companies that offer credentialing support and compliance updates generally outperform those that focus solely on claims submission.
4. Top 5 mental health billing companies in Canada & Australia – Full Comparison Guide
In Canada, some of the best companies for mental health billing in 2025 include JCL Billing Services, MedBill Canada, and HealthPro Billing. These leading firms excel in meeting provincial compliance standards, ensuring accurate claims and timely reimbursements for mental health providers. In Australia, Medicare-focused partners like MedBill Pro and Aussie Medical Billing stand out for their expertise in telehealth billing and adherence to updated Medicare rules. These mental health billing companies offer transparent dashboards, quick turnaround times, and strong compliance support—making them ideal for both solo practitioners and large behavioral health enterprises. A full comparison of these companies highlights ROI growth, improved claim efficiency, and higher client satisfaction ratings.
5. How do billing companies for mental health improve lead generation and revenue growth?
Billing companies improve revenue growth by reducing denials, ensuring quicker reimbursements, and freeing providers to see more patients. Lead generation improves indirectly because satisfied patients refer others when billing is transparent and error-free. Some billing companies also integrate with marketing CRMs, helping practices analyze patient acquisition costs alongside revenue cycle performance. This dual approach enhances both new client acquisition and the retention of existing clients.
6. Checklist: What features to look for when choosing a billing company for psychologists and psychiatrists?
Key features include: dedicated mental health coding expertise, denial management systems, compliance updates, credentialing support, transparent reporting, and 24/7 customer service. Practices should also evaluate whether the company provides cloud-based dashboards, AI-driven analytics, and patient-friendly billing statements. Choosing a company with these features ensures higher ROI, fewer denials, and smoother patient experiences.
7. What are the benefits of using cloud-based mental health billing services for enterprises?
Cloud-based billing provides real-time claim tracking, compliance updates, and integration with EHRs. Enterprises benefit from multi-location access, automated denial alerts, and predictive analytics. The cloud also enhances data security, ensuring compliance with regulations such as HIPAA, GDPR, and PIPEDA. For enterprises with large teams, cloud billing reduces manual errors, speeds up reimbursements, and enables centralized financial oversight, all while lowering IT costs.
8. How do mental health billing companies handle denial management and reimbursement challenges?
Denial management is handled through root-cause analysis, predictive claim scrubbing, and proactive resubmissions. Top billing companies maintain dedicated denial teams that follow up with insurers until claims are approved and settled. They also track denial trends and implement provider training to prevent recurring issues. This proactive approach not only recovers lost revenue but also reduces denial rates by up to 40% over time.
9. What jobs and career opportunities exist in billing companies for behavioral health professionals?
Opportunities include billing specialists, coding experts, compliance officers, denial management analysts, credentialing coordinators, and account managers. As behavioral health billing grows, so does the demand for professionals with psychiatric coding expertise. These roles are available across the US, UK, Canada, and Australia, offering stable career paths with strong growth potential.
10. Which mental health billing services are best for small practices vs. large enterprises?
For small practices, Therapy Notes Billing and Kareo are cost-effective solutions that provide simple, integrated services. Large enterprises, on the other hand, benefit from NCDS and AdvancedMD, which offer dedicated teams, compliance monitoring, and multi-location dashboards. The key is matching the company’s scale and technology to the provider’s size and growth goals.
